Introduction
In this comprehensive section, we delve into the critical aspects of wound assessment—a cornerstone of effective healthcare. Explore the profound significance of accurate wound assessment, uncover the intricacies of adopting a holistic approach, learn to craft precise wound management plans, and gain clarity on the optimal frequency for conducting wound assessments. This knowledge equips healthcare professionals with the essential skills to provide optimal care and promote the healing process for their patients.
Why is wound assessment so important?
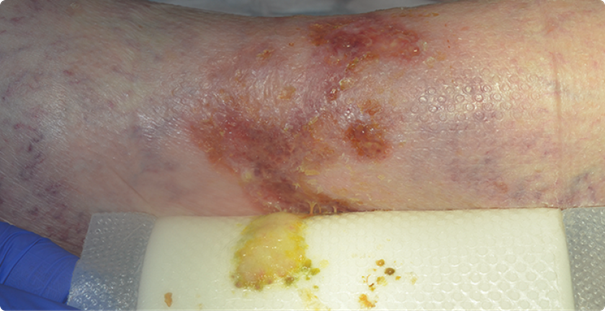
Living with a wound has a significant impact on a patient’s quality of life. As many of you know from your own clinical practice, non-healing wounds are not only painful; they also cause great distress for the patient.
Both patients and HCPs worry why the wound is taking so long to heal and what might be going wrong. Some have to deal with the smell of exudate, which might stop them from going out altogether – adding social isolation to their pain and distress.
Knowing how to assess the patient’s wound correctly is key in putting an end to their pain.
That means covering all the factors that affect the wound’s healing process – from identifying the underlying cause of the wound and the barriers that are preventing it from healing, to setting clear treatment goals and aligning expectations with the patient.
We call this approach holistic wound assessment. Let’s take a closer look at what that involves.
Why is holistic wound assessment?
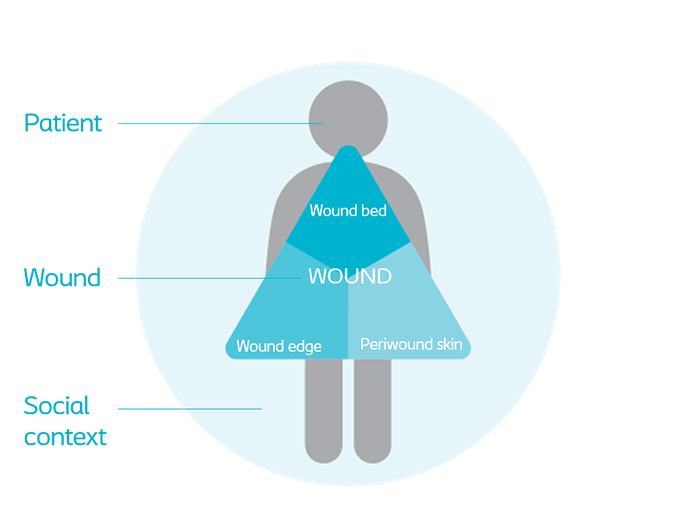
As the term suggests, a holistic wound assessment is an approach that takes into account the combination of factors – inside and outside the wound – that affect the healing process.
A holistic wound assessment involves:
- The patient’s medical history – including current and past medical conditions; their psychological, social and spiritual history; their wound care environment and access to specialised health services.
- A physical assessment of the patient - including factors such as respiration, blood pressure, heart sounds, skin assessment, etc.
- A comprehensive wound assessment – including assessment of the wound bed, the wound edges, the periwound skin and patient pain levels.
A structured approach to your wound care management plan
The holistic approach to wound assessment is a structured and comprehensive approach to wound management. It helps you to consider all the factors that affect wound healing and gives you a baseline for tracking the healing process so you can adjust the goals you set for management along the way.
With this approach, you are considering the ‘whole patient’ and not just the ‘hole in the patient’.
A wound assessment and documentation tool will help you to make sure you are conducting a holistic wound assessment. Check out our Triangle of Wound Assessment tool and let that guide you through the process.
Defining a management plan and treatment goals
Once you have done a comprehensive assessment of the patient and wound, you can move on to developing an effective wound management plan and set specific goals for the treatment.
Remember to involve your patient in this process. As you have probably already experienced yourself – and many studies have already documented – engaging patients directly in their care planning and treatment choices improves their adherence to treatment and ultimately ensures better outcomes.
A wound care management plan typically involves:
- Cleansing the wound;
- Debriding it of non-viable tissue (for example, necrosis and slough) to reduce risk of infection;
- Managing the moisture balance – rehydrating or reducing exudate levels to create a moist wound environment (for example by using an appropriate dressing);
- Protecting granulation/epithelial tissue;
- Improving the patient’s general wellbeing, by reducing pain and any smell coming from the wound.
The goals you set for the treatment of the wound will change over time as the wound starts to heal. But the only way you can keep track of the healing process is by assessing the wound frequently.
How often should you assess the wound?
A wound should be assessed at each dressing change – or at least once a week – to make sure the treatment is having the right effect.
It’s important that you set dressing change frequency against the treatment goals you have defined. For example, if you are managing a highly exuding wound, frequent weekly dressing changes will be necessary; if you are managing a granulating wound, you will usually only need to do a few dressing changes per week. Remember to document the reasons for how often the dressing needs to be changed.
If you observe any of the following:
- a less than a 20% improvement in the wound area over a period of four weeks;
- Unexpected increase in exudate;
- Suspected infection or biofilm;
- Increased pain or a general decline in the patient’s health and wellbeing
… you should always refer the patient to a specialist.
- Kennelly M, Thiruchelvam N, Averbeck MA et al., Adult neurogenic lower urinary tract dysfunction and intermittent catheterisation in a community setting: Risk factors model for urinary tract infections. Advances in Urology. 2019; Apr 2:1–13
- Islamoska S, Landauro MH, Zeeberg R et al., Patient-reported risk factors for urinary tract infections are associated with lower quality of life among users of clean intermittent catheterisation. Online survey; Edinburgh: BAUN poster; Nov. 2022 (PM-24180)
- Vasudeva P and Madersbacher H, Factors implicated in pathogenesis of urinary tract infections in neurogenic bladders: some revered, few forgotten, others ignored. Neurology and Urodynamics. 2014 Jan;33(1):95-100
